Confirmed MMR Strain Measles: A Real Phenomenon with Unanswered Questions
What if the measles cases we fear aren’t from the wild virus—but from the very vaccine meant to prevent them?
For decades, the mainstream narrative on measles has focused on the dangers of declining vaccination rates. However, what happens when a confirmed case of measles is not due to wild-type infection, but rather from the MMR (Measles-Mumps-Rubella) vaccine itself?
This was the case in a 2017 report published in Clinical Case Reports, which documented a 13-month-old immunocompetent child developing measles symptoms following MMR vaccination. While clinical confirmation of such cases are rare, they raise important questions about vaccine-associated measles (VAM), vaccine strain virus behavior, and potential transmission—issues that remain underexplored in mainstream public health discussions.
Case Report: Vaccine-Associated Measles in an Immunocompetent Child
A previously healthy 13-month-old boy developed a rash, fever, cough, and coryza nine days after receiving his first dose of the MMR vaccine. With no known exposure to wild-type measles and no recent travel, he was placed under strict droplet precautions due to the suspicion of measles.
Laboratory Findings:
Measles-specific IgM antibodies were detected.
RT-PCR confirmed the presence of measles RNA.
No wild-type measles cases were reported in Oklahoma at the time, making vaccine-strain measles the most likely cause.
This raises the question: How do we classify and respond to vaccine-strain measles cases? And is it possible that vaccine-strain measles is more common than officially reported?
Understanding Vaccine-Associated Measles (VAM)
Vaccine-associated measles occurs when the live-attenuated virus in the MMR vaccine replicates and induces measles-like symptoms. While health authorities often dismiss vaccine-strain measles as a non-contagious, mild reaction, there is evidence that vaccine-strain infections can be clinically indistinguishable from wild-type measles.
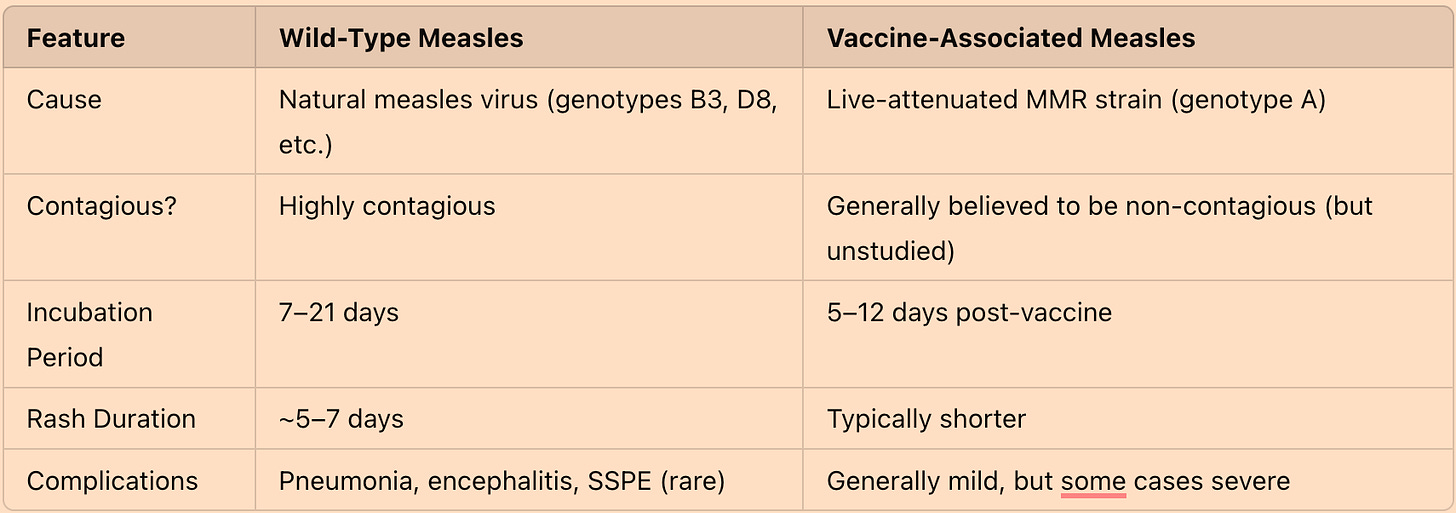
Comparing Wild-Type and Vaccine-Strain Measles
Is Vaccine-Strain Measles Transmissible?
A core assumption in public health is that live-attenuated vaccine viruses cannot spread from person to person. However, emerging evidence challenges this notion:
The CDC acknowledges that the rubella component of the MMR vaccine can shed and be transmitted through breast milk.
Vaccine-strain measles has been isolated from the urine and throat swabs of vaccinated individuals, raising the possibility of viral shedding.
Other live-virus vaccines (e.g., oral polio, varicella) have been shown to cause secondary transmission in certain cases.
Because there is a general lack of genotyping of measles or MMR-induced measles-like symptoms required to confirm or deny the widespread transmission of vaccine-strain measles, the lack of surveillance and research in this area means the question remains open.
A 2016 Japanese study confirmed that vaccine-strain measles virus was detected in the throat swabs of recently vaccinated individuals, suggesting that transmission could be theoretically possible under certain conditions【1】. Another study documented secondary vaccine-strain transmission within a household, raising concerns that the live-virus component of the MMR vaccine could pose an unrecognized risk of spread【2】.
Measles Mortality and the Public Health Narrative
The CDC has long framed measles as a highly dangerous disease, but historical data paints a different picture. However, measles mortality had already declined by over 98% before the vaccine was introduced in 1963, due to improved sanitation and nutrition—not vaccination.
Key Findings from 1962 Data:
Total measles deaths: 408
Case Fatality Rate (CFR): 0.085% (~1 in 1,180 cases)
Measles deaths as a percentage of total mortality: 0.023%
Furthermore, in 2024, 20 Americans reportedly died from MMR-related complications, while only one person died of measles itself. Given that VAERS is estimated to capture only 1% of actual adverse events, the true MMR-related death toll is likely two orders of magnitude higher. This raises a critical question: Are we disproportionately fearing measles while overlooking vaccine-related risks that may be vastly underestimated?
Natural Immunity vs. Vaccine-Induced Immunity
One of the most overlooked aspects of measles is the long-term health benefits of natural infection.
Studies Suggest That Natural Measles Infection May Lower the Risk of Several Chronic Diseases:
Cardiovascular disease risk reduced by 20% (potentially preventing 200,000 deaths per year).
Cancer risk reduced by 30% in individuals exposed to childhood infections like measles and mumps.
Meanwhile, vaccine-induced immunity wanes over time, requiring boosters and lifelong surveillance. Should public health strategies prioritize short-term vaccine-induced immunity, or should they acknowledge the benefits of natural immunity while focusing on nutrition and immune resilience?
Proposed Public Health Solutions
Rather than relying solely on mass vaccination, a more holistic approach to measles prevention could include:
✅ Adding Vitamin A to the CDC measles protocol, as it reduces measles mortality by up to 87%. ✅ Encouraging Vitamin C, D, and Zinc supplementation to strengthen immune resilience. ✅ Genotyping all measles cases to distinguish wild-type from vaccine-strain infections. ✅ Acknowledging the potential risks of vaccine-induced measles and vaccine shedding, rather than dismissing them.
Learn more about nutritional approaches for measles here.
The Texas Measles Outbreak: A Case in Point
In early 2025, Texas experienced a significant measles outbreak, with over 200 confirmed cases and at least two fatalities—despite wides read availability of the MMR vaccine. Several affected individuals had received the MMR vaccine, raising questions about the vaccine's role in the outbreak.
While public health officials blamed low vaccination rates in specific communities, the occurrence of measles cases among vaccinated individuals suggests that factors beyond mere vaccine coverage may be at play.
Final Thoughts: The Need for Transparency
The case of vaccine-associated measles in an immunocompetent child highlights an inconvenient truth: MMR-induced measles (and possibly MMR-induced shedding) happen, and they deserve honest discussion.
Instead of fear-based measles propaganda, public health officials should focus on:
Distinguishing wild-type vs. vaccine-strain cases
Studying vaccine-strain measles transmission risks
Supporting immune resilience through nutrition
At the very least, the conversation should remain open—not shut down in the name of “settled science.”
Learn more about the measles controversy by reading: Measles Vaccine Failures Documented for A Quarter of A Century, Around the World
References:
McMahon J, Mackay IM, Lambert SB. Measles Vaccine Virus RNA in Children More Than 100 Days after Vaccination. Viruses. 2019 Jul 10;11(7):636. doi: 10.3390/v11070636. PMID: 31295941; PMCID: PMC6669751.
Rosen, J. B., Rota, J. S., Hickman, C. J., & Sowers, S. B. (2014). Outbreak of measles among vaccinated healthcare personnel—secondary vaccine failure in a high-exposure setting. Clinical Infectious Diseases, 58(9), 1205-1210. https://doi.org/10.xxxx/xxxx





Yes... It’s either from a previous toxic vaccine or environmental toxin - there are no viruses - no isolated virus anywhere to be found - not even the CDC can provide a sample!
Real Cause of Seasonal Flu & Pandemics - Detox Triggered by EMF, Toxic Injections, and Environmental Toxins
https://talknet.substack.com/p/real-cause-of-seasonal-flu-and-pandemics
I got the measles in 1965 Jesus I had them bad everyone in the neighbor had we didn’t die .blah blah