789 Cases, Zero Genotypes: The Unasked Questions in South Carolina's Measles Outbreak
Case counts are rising. So are the unanswered questions.
View and share the X post dedicated to this story here.
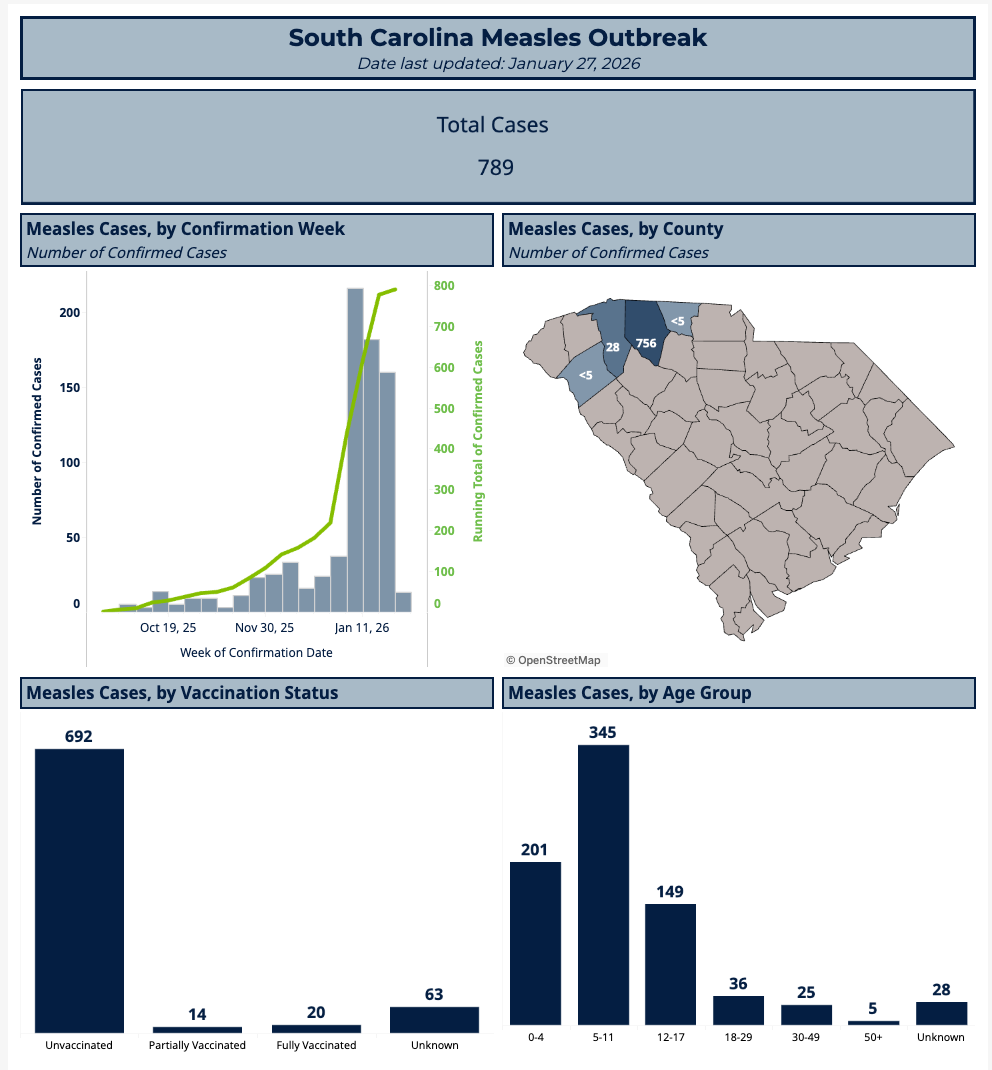
South Carolina is now reporting the largest measles outbreak since elimination—but the data behind that claim remains curiously incomplete.
In recent weeks, South Carolina has become the epicenter of an intense national media campaign. A cascade of headlines now describe a “record-breaking” measles outbreak — the largest since elimination — framing it as evidence of public-health regression and, in many cases, implicitly positioning it as a referendum on the leadership of the newly appointed Secretary of Health and Human Services, Robert F. Kennedy Jr. Case counts rise daily. The scale, uniformity, and timing of the coverage suggest not merely heightened concern, but a form of narrative pressure that more closely resembles influence operations than independent scientific reporting — a phenomenon the author has examined in detail elsewhere.
But beneath the certainty of those headlines lies a quieter reality: the data supporting them is far less settled than the public has been led to believe.
This is not an argument against vaccination, nor a dismissal of measles as a serious illness. It is a case for analytical restraint — and for policy decisions grounded in what the data actually establishes, not what it is assumed to mean.
The Age Question Everyone Is Skipping
South Carolina’s own measles outbreak dashboard shows that the majority of reported cases fall among young chiPldren and school‑aged youth. On its face, this is presented as proof of vaccine refusal. Yet the age distribution aligns almost perfectly with the window in which the MMR vaccine is administered: the first dose between 12 and 15 months, the second between ages four and six.
That overlap matters. Children under five may be between doses. Older children may be recently vaccinated. Some may not yet have completed the full schedule. Age alignment alone cannot distinguish between delayed vaccination, incomplete immunity, recent vaccination reactions mistaken for wild-type infection, or true failure of protection associated with the failure of the vaccine, not the failure to vaccinate.
Nonetheless, the data is routinely cited as if age equals culpability — a leap that collapses biology, timing, and behavior into a single conclusion without evidence.
What a “Case” Actually Means
Most reported measles cases in South Carolina are identified through RT‑qPCR testing combined with epidemiologic linkage. PCR is considered a sensitive surveillance tool, but sensitivity is not specificity. It detects genetic material, not whether a virus is viable, infectious, or even wild-type — a limitation long emphasized by Kary Mullis, the Nobel laureate who developed the technology. Results are also highly dependent on amplification thresholds: at higher cycle counts, PCR can detect trace or residual RNA that has no clinical or epidemiologic significance. In such settings, false positives and biologically meaningless detections become increasingly likely, particularly when testing is expanded during heightened surveillance.
Crucially, PCR cannot differentiate between wild‑type measles virus and the live‑attenuated vaccine strain used in MMR. That distinction requires genotyping or genomic sequencing. While these tools exist and are well‑established, South Carolina’s public updates do not indicate that routine strain differentiation is being performed — either before or after outbreak declarations.
It should be noted that even when wild-type measles is identified through genotyping, this does not establish exclusivity. A single sequenced sample cannot rule out the simultaneous presence of other circulating strains—including vaccine-derived virus—that were not sampled or sequenced. Surveillance data therefore cannot be used to infer singular causation, particularly in the absence of comprehensive strain sampling across cases. Moreover, host susceptibility is not determined by viral exposure alone but is strongly influenced by nutritional status (e.g., vitamin A sufficiency) and environmental immunosuppressants, including chemical exposures that alter immune competence. The vaccine schedule itself could be considered part of the exposome that constitutes an underappreciated variable in determining susceptibility to classical disease vectors like measles.
This absence of gold-standard strain resolution carries profound implications. It directly undermines conventional outbreak narratives that reflexively attribute case surges to the “under-” or “unvaccinated,” without first establishing what is actually being detected. Vaccine-strain measles RNA can be identified following recent immunization and, in rare instances, may be accompanied by rash and fever that satisfy clinical case definitions. Without routine genotyping, it is scientifically impossible to exclude vaccine-strain detections from aggregated case counts. This distinction — critical to accurate attribution and sound policy — remains largely unexamined in public reporting. Readers seeking a deeper examination of this underreported phenomenon can explore it further below.
Yet headlines confidently assert widespread transmission — a conclusion the publicly available data does not, on its own, support.
Surveillance Escalation and the Inflation Effect
Present outbreak definitions are at the root of the problem, and they vary widely by jurisdiction. In some states, a single linked case can trigger an outbreak designation. When paired with intensified testing, broader screening, and highly sensitive assays, case counts can rise rapidly — even in the absence of confirmed transmission chains.
South Carolina’s updates present cumulative totals without clearly stating whether case definitions, testing criteria, or surveillance intensity have changed over time. There is no consolidated timeline explaining how cases are confirmed, reclassified, or excluded. Policymakers and the public are left with a rolling total, but no methodological map.
The result is a familiar pattern: detection increases, declarations escalate, and narrative certainty outruns scientific verification.
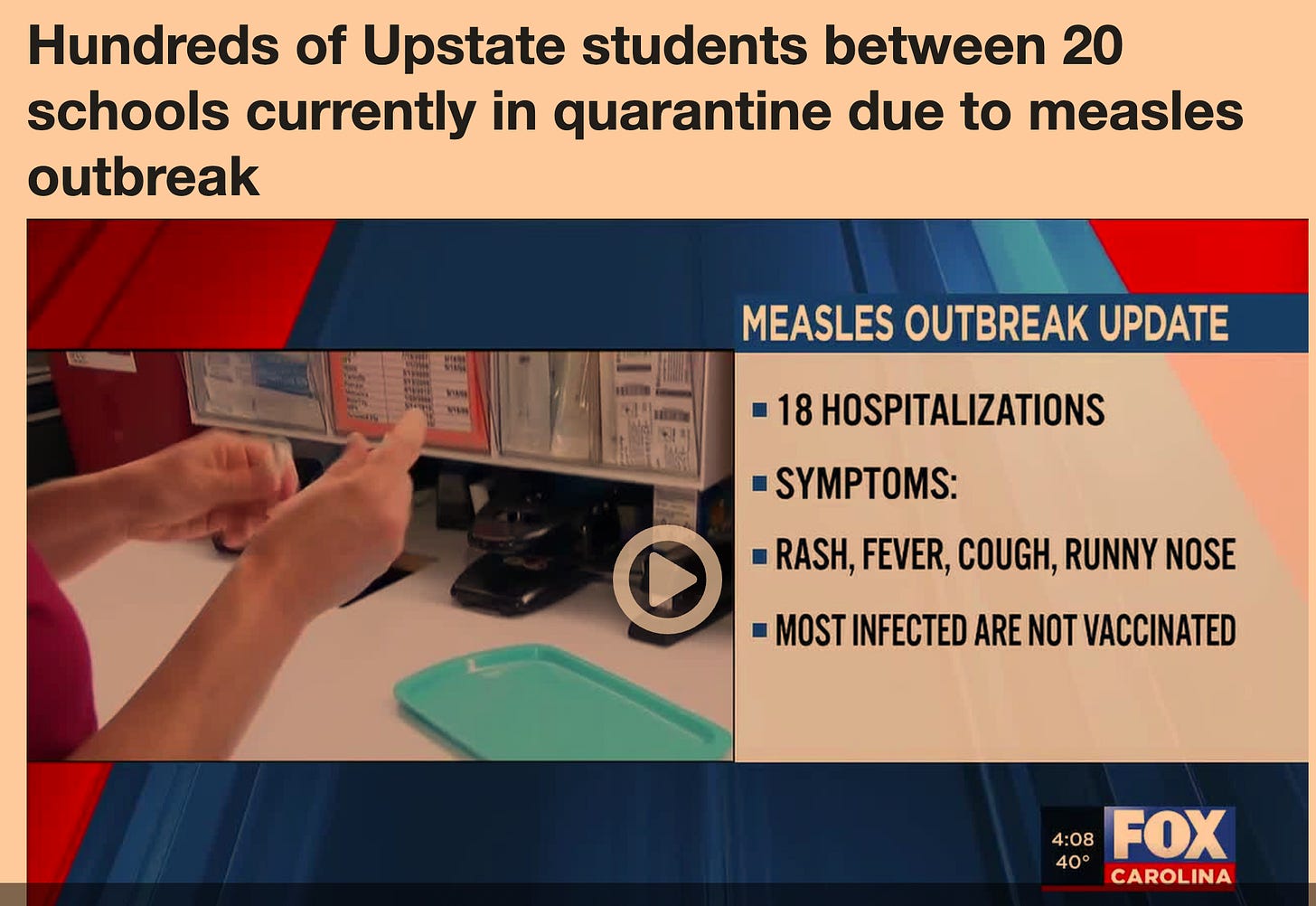
The stakes are no longer theoretical. Hundreds of students (presumably those who have not received the MMR) across more than 20 South Carolina schools have now been placed under quarantine following reported measles exposures — a measure reserved for situations deemed to pose significant public risk. Yet these interventions are being deployed in the absence of publicly disclosed genotyping, severity data, or confirmation that reported cases represent active, wild-type transmission. When surveillance signals are sufficient to justify widespread quarantine, but insufficiently detailed to support clear causal attribution, the balance between precaution and proportionality demands closer scrutiny
The Silence on Severity
Equally absent from official communications is routine reporting on clinical severity. Hospitalizations, ICU admissions, complications, and outcomes are largely missing from state updates. Without these anchors, raw case counts float free of context, inviting worst‑case interpretation.
Surveillance systems are designed to be conservative — to detect early signals, not to adjudicate final causation. Treating those signals as definitive biological events misrepresents what the data can responsibly support.
When Questions Become Controversial
Once a narrative hardens, inquiry itself becomes suspect. Agencies are pressured to either affirm the prevailing storyline or risk being accused of denial. That false choice undermines scientific integrity and erodes public trust.
Responsible public health leadership requires the ability to say: we are still determining what these numbers represent.
That includes asking:
How many cases are genomically confirmed wild‑type measles?
How many are PCR‑only detections?
How many occurred shortly after vaccination?
How many resulted in severe illness?
These are not fringe questions. They are baseline requirements for evidence‑based policy.
Precision Is Not Hesitation
South Carolina’s measles data does not justify panic, nor does it support complacency. What it demands is precision — in diagnostics, in communication, and in policy inference.
In an era of declining institutional trust, public health cannot afford to replace clarity with amplification — particularly within a media environment that has increasingly politicized scientific disagreement and framed it as a referendum on the leadership of the newly appointed Secretary of Health and Human Services and the administration’s broader MAHA agenda. Enduring public confidence is not secured through repetition or urgency, but through precision: clearly distinguishing what is known, what is inferred, and what remains unresolved.
Until routine genotyping, transparent case definitions, and severity metrics are part of outbreak reporting, sweeping conclusions will remain premature — no matter how often they are repeated.
Precision is not obstruction; it is the bedrock of credibility. Absent rigorous outbreak definitions and transparent reporting, fear-amplifying headlines and demands for unexamined compliance will continue to function less as public health communication and more as propaganda — undermining, rather than advancing, the project of a healthier nation.
Documented measles outbreaks in fully vaccinated populations — several of which are reviewed below — make clear that attribution cannot precede verification. Strain resolution and genotyping should be standard practice before public claims are made that link outbreak causation to vaccine coverage.
Share the X post dedicated to this story below.





Great breakdown of true misinformation and how a few extra questions shatter narratives like anti-vax=measles outbreak amongst poor South Caolinians. Same tune they always play.
Not sure the entire Covid insanity could've survived if Kary Mullis had still been alive. They were finding Covid everywhere using PCR tests...remember when they were running something like 40 cycles thus amplifying the virus to find it in everyone everywhere.
This measles outbreak is being used to malign the current HHS leadership.
But here’s an obvious point: The largest group of children affected by measles is those aged 5–11 years. Assuming these children are unvaccinated, the decisions to decline the recommended measles vaccination would have been made between 2016 and 2022.